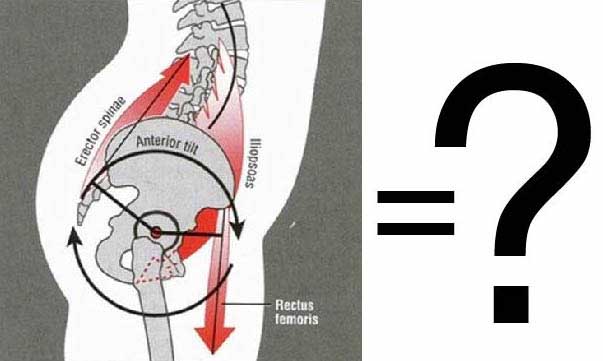
Opinions on what constitutes a pelvic problem abound. The term "forward pelvis" with its negative connotation, has come to be used for an assortment of pelvic / lumbar architectures, some of which, according to the Gokhale Method - are good, and some bad.
Have you been diagnosed with “forward pelvis” (aka “anterior pelvic tilt”)? If so, you may be concerned about the Gokhale Method recommendation to antevert your pelvis, thinking that this will exacerbate the problem.
Your confusion is not unique. Very few professionals, whether doctors, trainers, or wellness practitioners, differentiate between “forward pelvis / anterior pelvic tilt” and healthy pelvic anteversion. This can lead to poor recommendations like tucking your pelvis or doing crunches.

A common approach to fixing pelvic problems in modern times is the pelvic tuck and crunches, both of which carry significant risks. The Gokhale Method has different (and we believe better) solutions to various pelvic or lumbar issues that students may have.
Anterior rotation of the pelvis on its own is not the problem. It’s where else you rotate and how that marks the critical difference between a happy and an unhappy spine.
“Forward pelvis” is vague terminology that is used to describe a variety of spinal architectures that share the common (and not very revealing) element that the pelvis is inclined forward relative to the ground. The term does not distinguish between curves that occur high in the lumbar spine, which are liable to cause pain and dysfunction, and the curve that happens at L5-S1 which is normal and healthy.
Healthy pelvic anteversion occurs only between the lowest of the free vertebrae in a human spine (known as L5), and the top of the sacrum (known as S1). If the L5-S1 angle is intact, it’s possible to stack the entire vertebral column with little effort.
With a "Forward pelvis”, the rotation is not necessarily isolated at L5-S1—in fact, there may be no rotation at all at that point—and usually there is rotation at one or more adjacent vertebrae.
Curvature at L5-S1 and lumbar region | Upper lumbar curvature; none at L5-S1 | Curvature solely at L5-S1 |
|
|
|
Arthur White, MD, The Posture Prescription | ©2016 Gokhale Method |
In the Gokhale Method Foundations course, students work with a teacher to find a suitably shaped wedge to support their particular L5-S1 architecture. Once students learn how to sit with an appropriately rotated pelvis, they are often surprised by how effortlessly they can now remain upright. With the pelvis properly anteverted, the rest of the spine stacks and the back muscles can actually relax.

Student Travis Dunn’s Before and After sitting pictures. Taking the Gokhale Method Foundations course helped him find a sweet spot that got rid of his longstanding back problem.
Even though this is how you sat naturally when you were quite small, it can take some coaching to release the muscles previously needed to work to hold you upright!
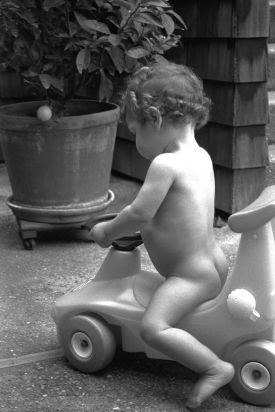
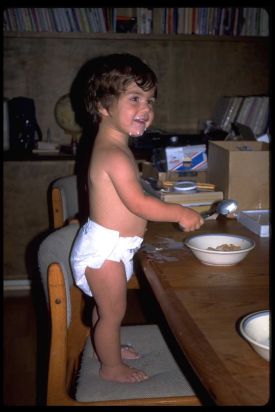
Nathan White (left), 1993, and Monisha White (right), 1996, displaying the natural and healthy pelvic anteversion shared by all young children. Notice that their pelvises tip forward in isolation from the lumbar spine.
What is unhealthy about most instances of “forward pelvis”? Let take a look at the physiology of the spine. Your vertebrae are cylindrical bones and in between each vertebra is an equally cylindrical disc that functions as a shock absorber.

Your spinal discs are shock absorbers. Most spinal discs are cylindrical in shape.
The L5-S1 disc at the bottom of the stack is unique among spinal discs in being wedge-shaped, with the broad edge of the wedge toward the front of the body. If you arch the spine, each cylindrical disc is forced into a wedge shape. Likewise, if the proper anteversion is not achieved at L5-S1, and there is some degree of tucking of the pelvis, the naturally wedge-shaped L5-S1 disc gets pinched into a more cylindrical form. After years of distorting discs in this way, you can expect degeneration, loss of disc height, and potential impingement of the corresponding spinal nerves.


When the cylindrical shape of the upper lumbar discs is not respected (left), or the wedge shape of the L5-S1 disc is not respected, there is compression, disc degeneration, and eventually pain and dysfunction.
With a return to correct anteversion of the pelvis (and a well-stacked spine), the cylindrical lumbar discs fit cleanly between the cylindrical vertebrae, and the wedge-shaped L5-S1 disc is given its own wedge-shaped space to call home. In this arrangement, the intervertebral discs can properly perform their shock absorber function while maintaining plenty of room for the segmental nerves to exit without compromise.

Well aligned vertebrae allow the spinal discs to perform their shock-absorbing function without compromise.
If you suffer from the variant of “forward pelvis” that includes problematic positioning of higher lumbar vertebrae, this can be caused by several things, each of which requires a different solution. If you are tensing the erector spine muscles (thrusting the buttocks backward or the chest forward), then the solution is to implement techniques to relax those muscles. Massage, stretching, and roller work are all good options. If the problem is a lack of tone in the abdominal wall, then you’ll want to seek out exercises to engage and strengthen the appropriate abdominal muscles.
It benefits pretty much everyone to find a healthy and natural curve at L5/S1 by sitting on a wedge to help tip the pelvis—and only the pelvis—forward, removing any counterproductive muscle tension. We have more detailed descriptions of how to properly “seat” your pelvis between your legs in our book, 8 Steps to a Pain Free Back.

It benefits almost everybody to use a wedge to help tip the pelvis - and only the pelvis - forward. This allows the vertebrae above to stack well without unhealthy muscle tension.
The lumbo-pelvic-hip-complex is made up of 15 bones and 29 muscles. With this many moving parts and a general lack of understanding about ideal human form, it’s no wonder that confusing and contradictory information abounds. Our aim is to shepherd you beyond non-specific descriptions of the pelvic area, and guide you towards healthy pelvic anteversion. This can go a long way toward resolving any low back pain and discomfort you have.
Join us in an upcoming Free Workshop (online or in person).
Find a Foundations Course in your area to get the full training on the Gokhale Method!
We also offer in person or online Initial Consultations with any of our qualified Gokhale Method teachers.





Comments
First thank you so, so much
First thank you so, so much for adding the list o' links to your emailed newsletter. Since I get only plain-text emails, I can now actually read your news!
Second, great article on anteversion. I am now using a 'saddle' stool at the computer and workbench, which provides both anteversion of the pelvis and 'opening' of the hip joint. (It also almost *prevents* slumping! Who knew?!) Any comments on saddle stools for those who can't afford your chair? (I have never used a backrest, so the cushion doesn't suit either.)
Warmly,
Elenor
Saddle stools are a big
Saddle stools are a big improvement on most chairs. I like them for short periods of sitting. Like you point out, they support pelvic anteversion and external leg rotation, which is huge. The challenges with saddle stools are:
I do recommend changing position frequently - my preference is stretchsitting (who can't use some extra stretch in their spine?), stacksitting (on a slope tailored to your pevlis), standing, samba, walking around, exercising, lying down. No chair does all that for you - it's you that needs to get up and move around - but I do like my chair to stretchsit and stacksit me.
This is a very interesting
This is a very interesting post as it's very easy to confuse swaying with proper anteversion. Would you expand on why crunches should be avoided? Can you point me to a list of your favorite core exercises that should be done regularly?
Many thanks.
Blake
"Crunches" are well-named -
"Crunches" are well-named - they crunch your discs and your spinal nerves! Situps have been weeded out of the Canadian Armed Forces regimen. My prediction is that crunches will be next for similar reasons. Here's a discussion of the subject: http://blog.bonati.com/us-army-phasing-out-sit-ups-due-to-spine-injuries/
Where is the evidence for the
Where is the evidence for the socalled j spine's existence?
If you mean "did you just
If you mean "did you just make up the name 'J-Spine'", the answer is yes. But the phenomenon it's describing abounds in old art, old photos, young children and non-industrial cultures (see the photos in 8 Steps to a Pain-Free Back)
If you mean do people with less upper lumbar curvature and more lower lumbar curvature (what I'm calling a J-Spine) have advantages over people who have more upper lumbar curve and less lower lumbar curve (what is commonly called an S-shaped spine), the answer is yes - they have less back pain. See the study by Jackson and McManus here: http://www.ncbi.nlm.nih.gov/pubmed/7939998
We need language to differentiate between upper from lower lumbar curve. Most studies in the medical literature concerning spinal curvature simply lump all lumbar curve together indiscriminately. My students find "J-Spine" and "S-Spine" handy terms to make the necessary distinction. I'd love to hear other ideas /language for talking about this.
Hope to be there in Everet,
Hope to be there in Everet, Washington. Thank you for the update .
This is coming from a purely
This is coming from a purely chiopractic perspective. The most subluxated segment in the low back is L5, and when it moves posterior (closing down the IVF where the nerves pass thru), the pelvic biomechanics will shift. Here's a link to the pre and post xray and video of severe anterior rotation of the pelvis. http://gohlclinic.com/prepost-xray-corrected-anterior-pelvic-tilt-video/ Anterior rotation of the pelvis will show a shorter ilium on the xray, since xrays are really just shadows. Also the obturators will be seen as smaller, explained in the video. Once we began correcting the subluxation at L5, the pelvis rotated posteriorly, lengthen the ilium shadow and the making the obturators larger. The anterior rotation of the pelvis wasn't the issue, the L5/S1 disc subluxation was. Stretching can't correct the subluxation. However proper posture can put less pressure on the discs, therefore causing less nerve pressure.
The J spine makes sense. This is very different in my profession where many believe the ideal spine presented by CBP is correct. The CBP model is based on mathematics, not how life works. It seems to me we should get our models for posture of the spinal column off of people from the past, and not in a mathematical laboratory. In the work at the clinic as people get their subluxations corrected, it seems they move more towards a flatter spine as you propose compared to the CBP ideal spine.
Thanks for perspective - it's
Thanks for providing a chiro's perspective - it's great to hear a different slant on this topic!
Thanks, Esther! Fascinating
Thanks, Esther! Fascinating article. I'm enjoying the discussion in the comments as well.
Best,
Michael
It's so nice to be
It's so nice to be communicating with people I know and value through my blog!
Thanks for posting this
Thanks for posting this article. The diagram of the forward pelvis on the top of the page/article looks almost just like mine! I've been concerned about my pelvis tilt and any possible stress on my lower back because of it. But basically you are saying it's not necessarily a problem in and of itself, but how I rotate, sit, etc.? And by rotate, do you mean the curve in someone's back?
I suppose the individual instruction in a seminar would be the best place to know what is best for me; I've read your book and I apply your principals to the best of my ability, however I understand we are all a little different in how it is applied, as you mentioned in this article. Also, I'm 5'0" short, so most chairs are too big for me - another sitting challenge. Pillows, towels, makeshift back-of-chair "filler" and traction ... fun stuff. :)
Thanks again!
The picture at the top of
The picture at the top of this article shows a sway back. The first step to improve this architecture would be to gently lengthen and reduce the excessive curve at L4-5 and above. You want to do this not in the usual way of tucking the pelvis, but rather, by "tucking" the rib cage.
It's true that the best way to learn this, as with any kinesthetic endeavor, is to learn hands-on from a qualified teacher. Think about how you would want to learn to play tennis or golf - walking, bending, sitting, and lifting are every bit as nuanced and are also best learnt from a coach. We offer Free Workshops in many locations and online to get you started; the Gokhale Method Foundations course is the best place to learn the basics that are covered in 8 Steps to a Pain-Free Back. Good luck!
How do your tilt
How do your tilt recommendations change for me, who has had a spinal fusion at L5-S1 3 years ago, due to spondylolisthesis (a 50% slippage, causing severe sciatica)? By the way I now have the resulting SI pain that I'm told often follows fusions, in addition to a lot of residual sciatic pain. I guess there was an adhesion on my crimped spinal cord.
1. Never fight metal!2.
1. Never fight metal!
2. Consider that juncture amply protected.
3. Work on using your movement habits to protect the joints around the fused portion of your spine. In your case, the SI joints and L4-5 (and higher ) will need extra protection.
4. The inner corset becomes even more important than usual in your situation. Make sure it is really strong and that you can cue it in a trice. Practice it and do extra exercises that include it (swimming may be an especially good choice if it appeals).
5. Depending on how your L5-S1 fusion was done (curve or no?), you may need to challenge yourself to do some degree of inner corset most of the time. If your base cannot be ideally positioned, you may not have the option to be relaxed and upright. But don't take this negatively - determine that you are going to become superstrong and you will not only mitigate your challenge but prevent all sorts of other problems from happening as well. Turn your challenge into a positive!
Hi. I recently had a full
Hi. I recently had a full hysterectomy and am wondering if there are any modifications to your methods of walking and sitting that I should make to protect my pelvic floor ? I’ve read about the possibility of prolapse and want to do what I can to prevent it from happening. Related to my question about posture, are there any specific exercises that you do and do not recommend for me ? I am otherwise an active, fit person in my early 60s. Thanks !
Since this pelvic position
Since this pelvic position (eventually) positions your pubic bones under your pelvic organs, this should help against pelvic organ prolapse and undue pressure on your pelvic floor.
I would caution against exercises which abruptly increase abdominal pressure, and also exercises that put downward pressure on the pelvic floor (like running, jumping, bouncing, and some dancing), to the extent those cause discomfort, especially when you are still healing from your surgery.
Beyond that, I think you need guidance that is customized to your particular architecture - I recommend working with one of our teachers as well as a PT together.
I always tried to seat the
I always tried to seat the way you describe here, but it causes me pain below the scapula. Is it normal till we get our bodies used to it or is there a chance I am doing something wrong?
In my philosophy, if it hurts
In my philosophy, if it hurts, it's wrong by definition. Pain is nature's way of telling you to try something different.
In my experience, it's challenging for most people to follow kinesthetic directions from a book. It's like learning to play golf from a book - you can learn some useful things, but at some point, you want a coach. Sitting, standing, walking, and other human motions are every bit as complex as a golf swing. There are many nuances to learn. I recomnend you either sign up for an initial consultation with one a teacher near you, or go to one of the free workshops that our teachers offer, or be courageous and sign up for the Gokhale Method Foundations course.
Hello.
Hello.
First of all, congratulations for your beautiful work. I have been practicing yoga for more than ten years and I have been diagnosed recently with herniation disc L5 S1. At the same time I have been having some problems with urine incontinence.
Our yoga method is focused on lengthen the spine as much as possible from the top to the sacrum. First, we try to erase the cervical curve by avoiding neck hiperextension (the chin never up). At the same time we take the chest out and we tuck the rib cage. finally we also do the pelvis retroversion so the spine is aligned. I guess because of this intense and continuos retroversion I have had this herniation. It makes sense.
My question is: Is it possible to work the same method and just ignore the retroversion? Or maybe it could cause more problems. Now I have introduced on my yoga sessions anteversion and also cobra posture with a little bit of neck extension but I do not know if it the right thing.
Could it be that by lengthen the spine all the way thorugh except the pelvis one provokes like a gap between the pelvis and the spine? It is difficult to me to understand how to work on lengthen the upper limb curvature but not the second one..
Sorry for my english I am from Spain
It would be great if you answer as this herniation has really confused myself.
Regards
This needs a qualified
This needs a qualified teacher. Finding the right amount of anteversion for a student is like trying to balance stones on each other. And then there's some serous pathology in the mix (a disc herniation) - I would be irresponsible in advising you to experiment in the way you are describing.
For what it's worth I will be in Valencia at the end of May and will be teaching our course and seeing a few students privately. If you are interested, write to [email protected] and let them know to keep you posted.
Critically thinking, if
Critically thinking, if someone has a tucked pelvis, then why stretch the low back? Isn't it because of short (and weak) abs and hams. The only reason the low back is cramped is because the glute medius doesn't work and the low back compensates for it. The stretch only feels good after the tip occurs.
But how do you get there? Do the hamstring muscles hamper getting the first tilt, since many back patients have chronically inactive hams (even when standing) but they still pull the sitbones with that thin, cordlike muscle. I'm getting an odd feeling in my abs, like I don't know which muscle is short and which one is overlengthened (or where the muscles even attach, although I know that). How do I get rid of this feeling? I suppose the stabilization doesn't work without a good spinal posture or 'stacking'.
So, is this really the first step in chronic rehab or is there even a lower level one could start with? And then what is the next step after the Gokhale Method?
I believe, that this
I believe, that this information will be mostly interesting for women. Although, I was also fascinated, while reading it. Thank you.
I have instability in L5-S1
I have instability in L5-S1 and I recently learned about the "Muscle Energy Technique" for adjusting the SI joint, hamstrings psoas, etc. Have you heard of this work? It seems compatible to the Gokhale method. I worked with a practitioner of the Hendrickson method, which incorporates MET. http://www.candacepalmerlee.com/
Thoughts? It appears easier to stacksit and tallstand now that the SI joint is unstuck. Before, when I tried to do these Gokhale postures, it was really painful.
Please advise. I just took the pop-up course two weeks ago and am trying my best to live these postures in everyday life. So much so that now, the old way of sitting doesn't work :)
However, I still get stuck with pain, as so many of my muscles turn on when I try to do simple movements. I wonder if others have this same issue?
Forward pelvic leads to many
Forward pelvic leads to many disabilities such as back pain which may be acute or chronic, spondylolisthesis, or PIVD. You may notice different postural alignment with the pelvic tilt.
There are be some treatment that reduces the chances of forwarding pelvic tilt is postural change, Recliners or ergonomic chairs for back pain, braces, etc.
Physical therapy also helps in reducing the forward pelvic tilt in early stages but in the later stage, surgery may be helpful.